Hepatitis C
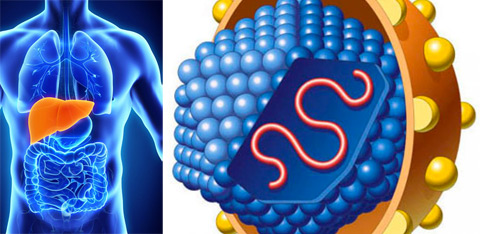 Hepatitis C is an inflammatory liver disease caused by hepatitis C virus (also referred to as HCV or hcv). Of the six types of known hepatitis viruses (A, B, C, D, E, and the recently identified G), hepatitis C most commonly causes chronic hepatitis and is the most common reason for liver transplantation, even though hepatitis B is more prevalent. Hepatitis C is not commonly spontaneously eliminated because the hepatitis C virus changes frequently, eluding the immune system. The inflammatory immune response to hepatitis C virus contributes to fibrosis (liver scarring) and cirrhosis (permanent liver scarring and altered liver structure). Six distinct HCV genotypes and many subtypes exist; genotype 1 is most common in the United States.
Hepatitis C is an inflammatory liver disease caused by hepatitis C virus (also referred to as HCV or hcv). Of the six types of known hepatitis viruses (A, B, C, D, E, and the recently identified G), hepatitis C most commonly causes chronic hepatitis and is the most common reason for liver transplantation, even though hepatitis B is more prevalent. Hepatitis C is not commonly spontaneously eliminated because the hepatitis C virus changes frequently, eluding the immune system. The inflammatory immune response to hepatitis C virus contributes to fibrosis (liver scarring) and cirrhosis (permanent liver scarring and altered liver structure). Six distinct HCV genotypes and many subtypes exist; genotype 1 is most common in the United States.
What are the risk factors and causes of hepatitis C?
Hepatitis C infection results from exposure to blood contaminated with hepatitis C virus, which replicates in liver hepatocytes. The hepatitis C virus can live on surfaces for 16 hours and possibly up to 4 days. Thus, those at high risk of contracting hepatitis C include:
- People who received blood transfusions or organ transplants before July 1992 (before blood pools were screened by polymerase chain reaction or PCR)
- People who received clotting factors before 1987
- People who received kidney dialysis
- Illicit peripheral drug users
- Health care workers at risk of needle sticks or eye splashes with HCV contaminated blood
- Children born to HCV positive mothers (caesarean section decreases this risk)
What are the symptoms of hepatitis C?
- Jaundice
- Mild fever
- Muscle and joint aches
- Nausea, vomiting
- Loss of appetite
- Abdominal pain
Hepatitis C infection is usually asymptomatic in its earliest stages. The incubation period lasts from 2 to 26 weeks after infection and acute hepatitis C (the 2 to 3 year period after infection) may be associated with mild flu-like symptoms or no hepatitis C symptoms. Chronic hepatitis C may not cause symptoms or may cause nausea and vomiting, abdominal discomfort, fever, and weakness.
Chronic liver infections develop in 55 to 85% of cases, chronic liver disease develops in 70% of cases, and cirrhosis of the liver develops (over 20 to 30 years) in 5 to 20% of hepatitis C patients. Ultimately, 1 to 5% of hepatitis C patients die from chronic infection resulting in liver cancer or cirrhosis of the liver. Problems in other organs including mixed cryoglobulinemia and poyphyria cutanea tarda are related to immune response to hepatitis C virus.
How is hepatitis C diagnosed
Blood tests measure antibody to hepatitis C virus via the enzyme-linked immunosorbent assay (ELISA) or enhanced chemiluminescence immunoassay (CIA) and are confirmed by the recombinant radio-immunoblot assay (RIBA). Antibody may remain in the serum after clearance of hepatitis C virus, or alternatively, viral antibody may not be produced in some immunocompromised patients, and therefore, active infection is diagnosed by measurement of the hepatitis C virus in blood by polymerase chain reaction (PCR), which measures hepatitis C viral RNA. A qualitative PCR assay is sensitive enough to detect low levels of virus, while the quantitative PCR assay measures the amount or titer of viral RNA.
Viral titer is used to predict response to hepatitis c medication but not disease progression. Liver enzymes, primarily alanine aminotransferase or ALT, are measured after positive blood results. A high ALT level indicates liver inflammation and chronic liver disease. Findings of normal liver function should be rechecked several times over a 6 month period and then annually. The genotype of the hepatitis C virus is determined before therapy is begun. Liver biopsy results are used to determine the degree of inflammation, the stage of hepatitis C, chance of disease progression, and the prognosis.
How is hepatitis C treated
Acute hepatitis C treatment is largely nonexistent since acute hepatitis is often undetected. Some hepatitis C information suggests that interferon therapy may reduce the chance of progression to the chronic phase. The aim of hepatitis C medication is control of liver disease symptoms, improvement of liver function, prevention of cirrhosis of the liver and liver cancer, and optimally, cure. Hepatitis C medication is administered to willing patients abstaining from drug and alcohol use with elevated ALT levels (for at least 6 months), detected serum hepatitis C viral RNA, and liver disease.
Interferon alfa (Intron A, Roferon-A, Infergen) is a marginally effective (10 to 30% response rate) immune modulator administered to chronic hepatitis C patients. Ribavirin (Copegus, Rebetol, Virazole), an antiviral administered with interferon alfa, improves the response rate to 40%. The new treatment for hepatitis C is the combined therapy (Rebetron) of pegylated interferon (longer acting interferon sold under the trade names Pegintron and Pegasys) and ribavirin, which generates positive response in 50 to over 80% of hepatitis C patients, and is administered for 24 weeks in HCV patients with genotype 2 or 3 and for 48 weeks in patients with genotype 1. Lack of detection of hepatitis C virus by PCR 6 months after therapy may indicate cure.
Liver transplantation is performed in some patients with chronic hepatitis C; however, hepatitis C infection commonly recurs in the transplanted liver.
A new generation of hepatitis C medication targeting viral replication or other essential viral processes is in development. In addition, development of drugs to prevent fibrosis and cirrhosis is underway. A vaccine has not yet been developed for hepatitis C, possibly because research on the hepatitis C virus is constrained by the inability to culture the virus and because the chimpanzee is the only available animal model.
Take action against hepatitis C
Hepatitis C patients should refrain from drinking alcohol, should not take medications or herbs without physician approval, should see their physician regularly, and should be vaccinated against hepatitis A if liver damage is present. Furthermore, hepatitis C patients at high risk of developing hepatitis B, which is also transmitted via blood, should be vaccinated against hepatitis B. Precautions to minimize spread of hepatitis C include not sharing razors or toothbrushes with infected individuals.