Traveling while pregnant
 The safest time for traveling while pregnant is during the second trimester (18 through 24 weeks) when you are usually feeling your best and are in the least danger of experiencing a miscarriage or premature labor, according to the American College of Obstetrics and Gynecology.
The safest time for traveling while pregnant is during the second trimester (18 through 24 weeks) when you are usually feeling your best and are in the least danger of experiencing a miscarriage or premature labor, according to the American College of Obstetrics and Gynecology.
It’s generally advised that women in their third trimester should stay within 300 miles of home because of concerns about access to medical care in case of problems such as hypertension, phlebitis or false premature labor. When making the decision to travel, it’s important to consider the potential problems associated with international travel, as well as the quality of medical care available at your destination and during transit. It’s a good idea to consult with your health care provider before making any travel plans.
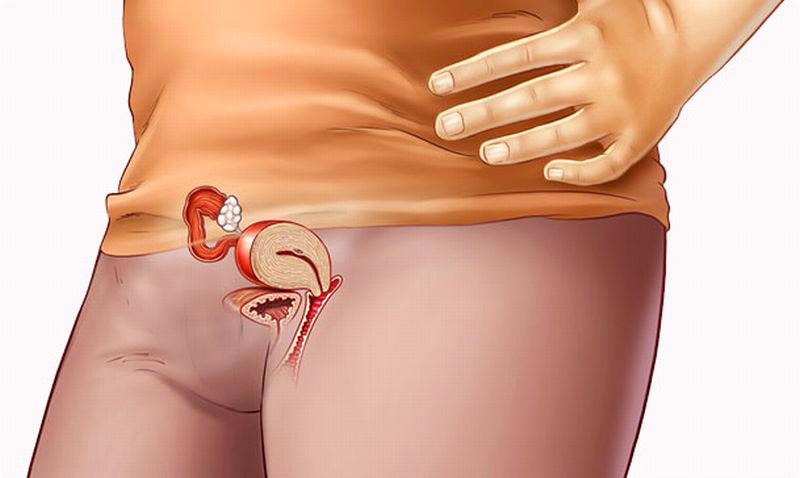
Typical problems that you might encounter are the same as those experienced by many pregnant women: fatigue, heartburn, indigestion, constipation, vaginal discharge, leg cramps, increased frequency of urination and hemorrhoids.
Symptoms that need immediate medical attention:
- bleeding,
- abdominal pain or cramping,
- passing of clots or tissue,
- contractions,
- ruptured membranes,
- excessive swelling of your legs,
- headaches.
Guidelines for the pregnant traveler
- Avoid potentially contaminated water and food. Pregnant travelers should eat only well-cooked meats and pasteurized dairy products, while avoiding preprepared salads. This will help to avoid diarrhea, as well as infections such as toxoplasmosis and listeria, which can cause serious problems during pregnancy.
- Don’t travel alone. It’s advised that you travel with at least one companion.
- Don’t miss your scheduled prenatal visits. Determine beforehand whether prenatal care will be required abroad and, if so, who will provide it.
- Take a close look at your health insurance coverage. Make sure before traveling that your health insurance is valid while abroad and during pregnancy, and that the policy covers a newborn should you give birth. Also, a supplemental travel insurance policy and a prepaid medical evacuation insurance policy should be obtained, though many may not cover pregnancy-related problems.
- Check into available medical facilities at your destination. For a woman in the third trimester, medical facilities should be able to manage complications of pregnancy and should be able to perform a cesarean section.
- Know your blood type.
Air travel during pregnancy
Commercial air travel poses no special risks to a healthy pregnant woman or her unborn baby.
If you’re looking for the most space and comfort you might want to request an aisle seat at the bulkhead, but a seat over the wing in the middle of the plane will give you the smoothest ride. Be sure to get up and walk every half hour during a smooth flight and flex and extend your ankles frequently to prevent phlebitis. The safety belt should always be fastened at the pelvic level. Bring along plenty of water to drink because of the dehydrating effect of the low humidity in aircraft cabins.

Each airline has policies regarding pregnancy and air travel. It is always safest to check with the airline when booking your reservations because some will require medical forms to be completed. Domestic travel is usually permitted until the pregnant traveler is in her 36th week of gestation and international travel may be permitted until the 32nd week. Be sure to carry documentation stating your expected due date.
Contraindications to flying include severe anemia (hemoglobin concentration below 7 grams per deciliter), sickle-cell disease or trait, a history of thrombophlebitis or placental problems; however, supplemental oxygen can be ordered in advance.
Travelers’ diarrhea
Pregnant travelers should eat only pasteurized dairy products and well-cooked meats, while avoiding preprepared salads. This will help to avoid diarrhea, as well as infections such as toxoplasmosis and listeria.
It is important to be careful about what you eat and drink when traveling during pregnancy because dehydration from travelers’ diarrhea can lead to problems with inadequate placental blood flow. It is important to boil potentially contaminated water. Pregnant women should be advised not to use prophylactic antibiotics for the prevention of traveler’s diarrhea.
Oral rehydration is the recommended therapy for traveler’s diarrhea. The combination of kaolin and pectin may be used, but loperamide should be used only when necessary. The antibiotic treatment of traveler’s diarrhea during pregnancy can be complicated. An oral third-generation cephalosporin may be the best option for treatment if an antibiotic is needed.
The pregnant traveler and vaccination
It is crucial to carefully review the risks and benefits of each immunization, because there are theoretical risks to your unborn baby from vaccination. Pregnant women, in general, should be advised to avoid live vaccines and to avoid becoming pregnant within 3 months of having received one.