Fetal fibronectin
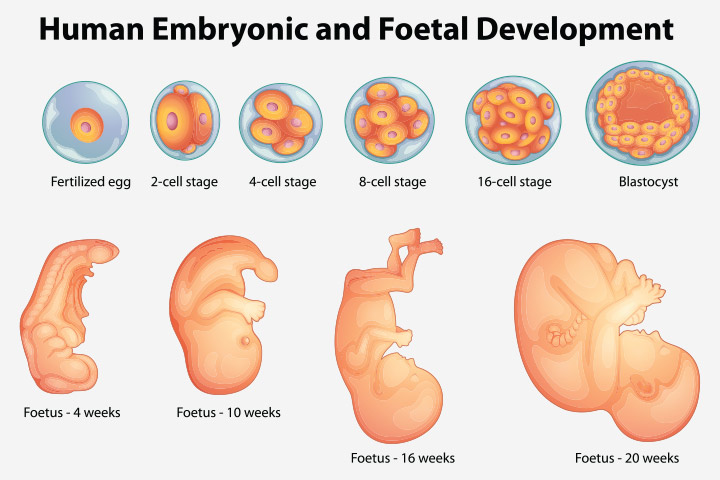
Fetal fibronectin is a large modular glycoprotein that helps bind cells in tissues and produced by the chorionic membrane. Fetal fibronectin (fFN) is located at the junction between the amniotic membranes and uterine side wall. Fibronectin shows profound effects on cell growth, adhesion, migration and differentiation. It plays a crucial role in embryogenesis by guiding cell attachment and migration during embryonic and fetal development.
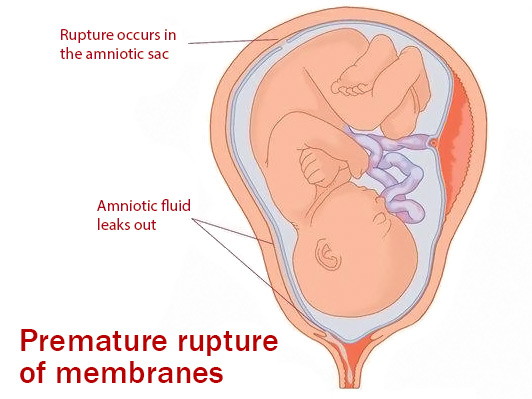
The fibronectin is present in high levels during pregnancy prior to twenty weeks, but then subsequently falls to low levels thereafter. It has been noted that fibronectin levels appear to rise two to three weeks prior to term delivery. It has also been noted that it has been found in vaginal swabs after 22 weeks only after compromise of the amniotic membranes.
Within the United States, premature birth is the single largest cause of perinatal morbidity and mortality. Over one million episodes of preterm labor occur annually in the United States with estimates of costs of greater than five billion dollars. Clinical variables currently available are extremely insensitive to accurately predict who will or will not deliver. Currently approaches to predict preterm labor have been based upon questionnaires which vaguely predict classification into high risk or low risk for delivery, signs or symptoms such as contractions, bleeding or dilatation of the cervix, or cervical ultrasound. The lack of an extremely sensitive marker leads to multiple episodes of admission for preterm labor. Fetal fibronectin test offers a new approach to the diagnosis of preterm labor.
Fetal fibronectin test
Currently, there is a rapid test for fetal fibronectin screening. With this test, clinical results may be available in as little as one hour. Much like when a Pap smear is performed, the patient presents to a physician’s office where a speculum is placed into the vagina. Thereafter, a simple Q tip is utilized to obtain vaginal secretions which are submitted for fetal fibronectin testing.
Within the United States, fetal fibronectin test can be used to assess the risk of preterm labor in women with signs and symptoms to further aid accuracy to their diagnosis. Fibronectin test may be used on patients who are from 24 to 34 weeks of gestation with intact amniotic membranes and dilatation of the cervix of less than 3 cm. In patients who present with signs and symptoms of preterm labor, only one out of 25 delivers in less than fourteen days. This leads to a large amount of over-treatment of preterm labor. Fetal fibronectin test can be used to further elucidate the risk of true preterm delivery in these patients.
Positive and negative results
For example, if a fetal fibronectin test result is negative in a patient presenting with symptoms and signs of preterm labor, the patient has only a 1 out of 125 chance of delivering within two weeks instead of the one in 25. If a fetal fibronectin test result is positive in the above patient population, they have a 1 in 6 chance of delivering within the next 2 weeks. In the patient population with negative fetal fibronectin tests, only 1 out of 12.5 will deliver at less than 37 weeks and if a fibronectin result is positive, one out of two will deliver at less than 37 weeks.
Utilizing a fetal fibronectin test, there is a dramatic affect upon patients being admitted for preterm labor symptoms. As stated above, fetal fibronectin tests in a study performed showed a reduced amount of admissions, decreased hospital stay, and decreased utilization of medications to stop uterine contractions. Additionally, there is no major negative impact on outcomes. Furthermore, there is a trend towards increased steroid use for infants that ultimately end up in the neonatal intensive care unit which provides improved outcome.
There is total reduction in admissions and charges per admission of approximately 55 percent in those patients who undergo fibronectin who are symptomatic for preterm labor. Hence, the proper use of fetal fibronectin may provide improved patient care to more accurately provide and assure a healthy outcome to the patient and her infant. It also appears to reduce costs of medical care which is becoming an issue of increased importance in today’s modern medical climate.