Hormone replacement therapy
Hormone replacement therapy (HRT) is a prescription drug therapy consisting of estrogen and progestin, two female hormones that a woman’s body stops producing at menopause. HRT can help reduce the symptoms associated with menopause.
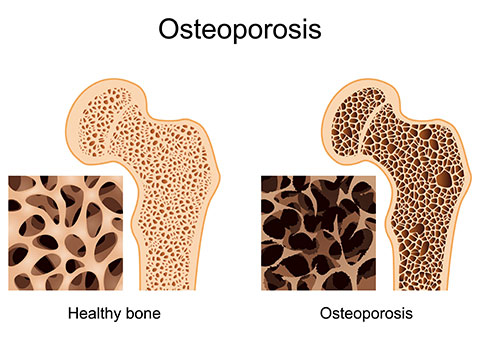
Menopause isn’t a disease but a natural part of aging. However, some women find the accompanying symptoms uncomfortable, even debilitating. Others are at higher-than-average risk for coronary heart disease or osteoporosis, and their declining estrogen levels only make matters worse. The good news is that there are medical treatments available that can offset both menopausal symptoms and rising disease risk. Women may take one or more of these hormone drugs in the form of pills, suppositories, skin patches, vaginal rings, creams or injections.
Since the 1940s, HRT has been offered to women primarily as a way to ease menopausal symptoms, such as hot flashes and vaginal dryness, resulting from declining estrogen levels. More recently, hormone therapy is also seen as a way to prevent chronic disease, even extend life. The term “replacement” therapy isn’t truly accurate since the therapy provides only a small amount of the estrogen normally produced by the ovary.
Benefits and risks of hormone replacement therapy
Many experts believe that the benefits of HRT may be greater than the risks, but scientists do not yet fully know the risks of long-term HRT. Most doctors will prescribe hormone therapy to women who’ve undergone surgical menopause before age 45. These women will live a longer time without the benefits of estrogen and so will have higher risks of heart disease and osteoporosis. Other women who may benefit are those at high risk of fractures because of other factors, such as long-term oral steroid use. And, finally, women whose menopausal symptoms are affecting their quality of life may want to consider hormone therapy. Symptoms may recur once treatment is stopped.
HRT can prevent – but not reverse – the bone loss at menopause that can contribute to osteoporosis. These medications can also help protect against colon cancer.
HRT also raises the level of “good” HDL cholesterol and lowers the level of “bad” LDL cholesterol, which, in theory, should lower the risk of heart disease. However, results from the Heart and Estrogen/Progestin Replacement Study (HERS), involving 2,763 postmenopausal women treated with an estrogen/progestin combination for approximately four years, found that HRT did not prevent further heart attacks or death from coronary heart disease. It also increased the risk of clots in the veins and lungs. There was a trend toward a higher risk of heart attacks in the first year of therapy, which was reversed during the final two years. The researchers speculate that the treatment may have lasted too short a time for its cholesterol-lowering effects to reduce the women’s heart-disease risk. We’ll have to wait for more studies before the risks and benefits of HRT to women with heart disease are fully understood.
HRT may increase the risk of breast cancer. Estrogen given without progestin – called estrogen replacement therapy, or ERT – raises the risk of uterine cancer. (Adding progestin protects against uterine cancer by keeping uterine cells from dividing.) Therapy using estrogen alone is usually reserved for women who’ve had their uterus removed and who therefore don’t need to worry about uterine cancer.
Though millions of women take HRT, it’s not the right choice for every woman. Many questions remain unanswered about HRT, and a woman must look closely at her own personal and family medical histories before deciding whether the side effects and risks of the therapy outweigh the benefits for her. Remember, HRT is not the only option for preventing disease. Changing your lifestyle – eating better, getting regular exercise – can also go a long way toward reducing your risk.
On the other hand, if a woman has heart disease, high blood pressure, diabetes, liver disease, blood clots, seizures, migraine headaches, gallbladder disease, or a history of cancer, she may not be the best candidate for HRT, but she may still benefit from the therapy as long as she is closely monitored by her physician. Since HRT may raise the risk of breast cancer, women who fear getting this disease may not feel comfortable taking it. Also, daughters of mothers who took diethylstilbestrol (DES) during pregnancy may have changes to their reproductive system that make HRT dangerous.
If you decide to take HRT, keep in mind that the regimen can be personalized – in terms of dosage, type, and frequency – for your individual needs.
Types of HRT
Estrogen can be taken in various forms, including pills or tablets, vaginal creams, vaginal rings, or patches that attach to the skin and release estrogen through the skin.
| Type of HRT | Drug brand name |
| Estrogen | Estratab, Gynediol, Estrace, Cenestin, Menest, Ogen, Premarin |
| Estrogen patches | Estraderm, Alora, FemPatch, Climara, Vivelle |
| Vaginal estrogen | Femring, Vagifem, Estring |
| Progestin | Provera, Cycrin |
| Natural progesterone | Prometrium |
Pills and tablets
Pills are the most widely prescribed form of HRT. The estrogen is usually conjugated equine estrogen, which comes from the urine of pregnant mares. Oral estrogen pills are usually taken daily for 25 days. The advantage of pills is their convenience and ease of use. While some of these pills must be taken with meals (they require fat to be absorbed), other are absorbed by placing them under your tongue.
Progestins are also prescribed mainly in pill form. (A transdermal patch is on the drawing board.) These pills are taken either for two weeks every month or in lower doses every day along with estrogen. A combination pill of conjugated estrogen and a progestin called medroxyprogesterone acetate is available.
For women who take the male hormone testosterone along with estrogen, there’s a combination pill available as well. Testosterone is sometimes prescribed to women who’ve had their ovaries removed and consequently experienced a drop in sex drive. However, studies on its ability to raise sex drive are mixed and getting the right dose is tricky: Too much can cause unwanted side effects, such as agitation or facial hair growth.
Skin patches
The transdermal estrogen patch, which resembles a half-dollar-sized Bandaid, is placed on the abdomen or lower back, where it continually releases a small amount of estrogen. Transdermal patches are used to ease menopausal symptoms and to prevent osteoporosis. (Their effectiveness in preventing heart disease is under study.) Patches are changed one or twice a week.
There are several advantages of the skin patch: Because estrogen is absorbed through the skin into the bloodstream, smaller doses can give the same benefits as estrogen pills. And by bypassing the liver, the estrogen is less likely to cause nausea or to worsen existing medical problems, such as gallstones or liver disease. As for side effects, the adhesive on the patch can irritate the skin and cause rashes. And in hot climates, women sometimes find that sweat interferes with the patch adhering well to skin.
Vaginal estrogen creams
Vaginal estrogen creams are intended for women whose chief complaints are vaginal irritation, dryness, itching, and painful intercourse. The creams, applied locally to vaginal tissues, are inserted into the vagina with an applicator several times a week. These creams are not appropriate for other menopausal symptoms, such as hot flashes, or for the prevention of osteoporosis or heart disease.
The advantage of the creams is that they pose less of a risk for women trying to limit their estrogen exposure. (If the recommended dose is exceeded, it’s possible for the estrogen to be absorbed into the bloodstream in amounts large enough to raise blood estrogen levels.) The disadvantage is that creams are messy.
Vaginal estrogen ring
Another option for treating vaginal dryness is the vaginal estrogen ring, which is inserted into the vagina like a diaphragm. The ring releases a continuous dose of estrogen for 90 days. The chief drawback is discomfort in the vagina and gastrointestinal tract.
HRT treatment regimens
Doctors may prescribe different schedules for taking HRT. With “cyclic hormone therapy,” women take estrogen for 25 days and a progestin pill for 10 to 14 days each month. They repeat the same pattern every month. This pattern often causes regular monthly bleeding like a menstrual period.
Some women take HRT every day of the month without any break. This pattern usually stops regular monthly bleeding. Talk with your doctor about the system that is best for you.
When should you begin HRT
How early a woman should start taking HRT depends on why she’s taking it. To ease menopausal symptoms, she may want to start taking it when symptoms become too uncomfortable. If she’s trying to cut her risk of heart disease, it might make sense to wait until around age 65, when a woman’s risk of heart disease typically rises. The use of hormone therapy immediately after menopause helps prevent the loss of bone due to estrogen deficiency, but even starting at age 65 will benefit bones.
Duration
Women taking HRT to relieve menopausal symptoms may need only a short course of estrogen (six months to two years). For women trying to lower their risk of disease, it’s less clear. Women at high risk of osteoporosis may need to take HRT indefinitely, as long as they don’t experience uncomfortable side effects. For women who’ve had a surgical menopause, most physicians prescribe estrogen therapy at least up to the time of a natural menopause.
According to the Nurses Health Study – a study that followed nearly 60,000 women over 16 years – taking HRT for a few years led to a lower overall death rate, mostly because of fewer deaths from heart disease. However, taking HRT for more than ten years cut this benefit by half because of more deaths from breast cancer.
Some researchers are now suggesting that women take “drug holidays” – that is, take estrogen for, say, five years, stop for six months, then start up again. Their reasoning: While therapy might offer protection to the heart, it gives breast cells a break from estrogen growth-stimulating effects. (Note: Never discontinue HRT all at once. Talk to your doctor about a regimen for gradual withdrawal.)
Side effects
As many as two-thirds of women who take HRT stop within two years, mostly because of undesirable side effects. Some women may experience vaginal bleeding, headaches, nausea, vaginal discharge, fluid retention, and swollen breasts. While some women complain of weight gain, there’s no evidence that the hormone therapy is to blame. One study, in fact, found that women taking HRT gained less weight than those not taking it. Women on HRT, however, are more likely than other women to have abnormal vaginal bleeding. If this happens to you, you’ll have to undergo medical tests – such as an endometrial biopsy or a dilation and curettage – to find the cause of the bleeding.
Oral contraceptives
Combination oral contraceptives contain estrogen and progestin, although in amounts five to ten times higher than in HRT. Like HRT, they can help ease hot flashes and vaginal drying and control irregular bleeding. Plus, they prevent pregnancy, if a woman is still fertile. If you’re taking the Pill for these symptoms, your doctor will periodically give you a follicle stimulating hormone (FSH) test to make sure you aren’t in menopause.
Other prescription alternatives
For women who can’t take estrogen (due to prior breast cancer, for example), other prescription drugs are available to ease menopausal symptoms such as hot flashes. Clonidine (Catapres), a drug typically used to treat high blood pressure, can relieve hot flashes in some women; it’s usually worn as a skin patch. Other drugs include belladonna (Bellergal) and megestrol acetate (Megace).
Working with your doctor
Before you decide about HRT, discuss the possible risks, benefits, and side effects with your doctor. Print out the decision chart and take it with you to your appointment. It can help you and your doctor get a handle on the benefits and risks of HRT for you. After reviewing it together, ask your doctor the following questions:
- What do you think are my long-term health risks, based on my personal and family medical histories?
- What are the reasons I should start HRT now, rather than waiting until later in life?
- Do you advise estrogen alone or in combination with progestin? Why?
- What form of HRT – pill, patch, ring – do you recommend? Why?
- What kinds of side effects can I expect?
- Are there any side effects that warrant immediate medical attention?
- How long do I need to take hormone replacement therapy?
- If I take HRT, what kind of regular follow-up care do I need?
- What percentage of your patients take HRT?
Be sure to let your doctor know all the prescription drugs you are taking, as well as any nutritional supplements or herbs.
Ongoing research regarding HRT
Research continues into the effects of hormone replacement therapy. For example:
- Clinical trials have shown antidepressants to be moderately effective in relieving symptoms associated with hot flashes. However, they have not yet been officially approved for this use. Soy products may also relieve symptoms because they contain an estrogen-like substance called phytoestrogen. However, this link has not been conclusively proven and the benefits of soy continue to be examined for women.
- Research continues into whether herbs (such as black cohosh), natural products and alternative medicine can help relieve symptoms associated with menopause.